03 Sai Tarun (july 24 2021)
GENERAL MEDICINE CASE (25-07-21)
Welcome and greetings to every one who are visiting my blog. This is A.Sai Tarun of 3rd semester. This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
Introduction
Patient was apparently asymptomatic for 6 days back then had sudden onset of fever , low grade hot.
HISTORY OF PAST ILLNESS
PERSONAL HISTORY
•Mixed diet
•Loss of appetite
•Sleep adequate
•Bowel and Bladder movements regular
TREATMENT HISTORY
FAMILY HISTORY
•Not significant
GENERAL EXAMINATION
•Patient is conscious, coherent and cooperative
•Moderately built and Moderately nourished
•No signs of - Pallor
Cyanosis
Clubbing
•Icterus present
VITALS
•Temperature - Afebrile
•PR - 80 bpm
•BP - 110/70 mmHg
SYSTEMIC EXAMINATION
•S1, S2 heard
•No murmurs
RESPIRATORY SYSTEM:
•NVBS heard
CENTRAL NERVOUS SYSTEM:
•Intact
•No focal defect
•No abnormality detected
INVESTIGATIONS
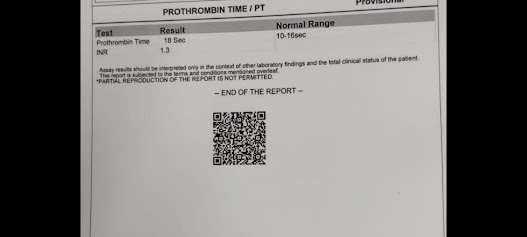
Prothrombin time
24/07/21
Complete blood picture
Complete urine examination









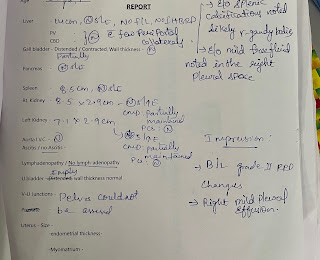


Comments
Post a Comment