03 Sai Tarun (24-08-21)
GENERAL MEDICINE CASE (24-08-21)
Welcome and greetings to every one who are visiting my blog. This is A.Sai Tarun of 3rd semester. This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
DATE OF ADMISSION - 20/08/21
Introduction
- A 32 year old male came to casuality with H/O pain abdomen in epigastric region since afternoon and 2 episodes of vomitings and giddiness since afternoon and fever from 1 day.
Chief complaints and Duration
-Patient was apparently asymptomatic till yesterday and had sudden onset abdominal discomfort and vomiting of 1 episode - non bilious, on projectile food as content with epigastric pain-thrombing type ,non radiation not associated with constipation or loose stools.
HISTORY OF PRESENT ILLNESS
-Fever :1 episode and Morning high grade associated with chills and rigor, no diurnal variation not associated with cold, cough, SOB, headache.
-Patient then went to MP with C/O vomitings and epigastric pain.
-Last binge of alcohol yesterday.
HISTORY OF PAST ILLNESS
-On presentation cold extremities + , pulse feeble, BP 70/40, and started on fluid resuscitation.
PERSONAL HISTORY
•Mixed diet
•Loss of appetite
•Sleep adequate
•Bowel and Bladder movements regular
•Regular alcohol drinker - 4times/day half quarter to 1 bottle since 20 yrs.
•(Tobacco)Kaini 1/day since 5yrs.
TREATMENT HISTORY
FAMILY HISTORY
• Father has H/O Diabetes.
GENERAL EXAMINATION
•Patient is conscious, coherent and cooperative
•Moderately built and Moderately nourished
•No signs of - Pallor
Cyanosis
Clubbing
Icterus
• Dehydration - Mild.
VITALS
•TEMP -99.4F
•Pulse rate -60bpm/low volume
•Respiratory rate - 12cpm
•BP- 70/40
•SPO2 - 97%
•GRBS - 96 mg%
SYSTEMIC EXAMINATION
•S1, S2 heard
•No murmurs
RESPIRATORY SYSTEM:
•NVBS heard
•Position of trachea - central
•Breath sounds - vesicular
ABDOMEN
•Shape - obese
•Tenderness in epigastric and hypochondrial region.
•No palpable mass
•No free fluid
•Spleen and liver not palpable
CENTRAL NERVOUS SYSTEM:
•Intact
•No focal defect
•No abnormality detected
•Glasgow scale 15/15
CEREBRAL SIGNS:
• No finger nose incordination
•No knee heel incordination.
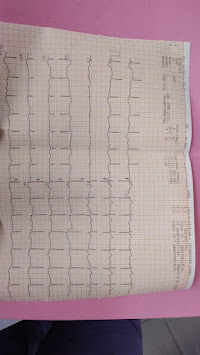
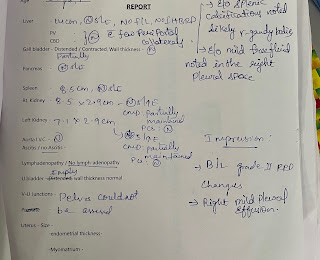
INVESTIGATIONS
PROVISIONAL DIAGNOSIS
TREATMENT
Rx
-Iv fluids NS and RL at 75 ml/hr
-INJ CEFTRIAXONE 1GM IV/BD
-INJ METROGYL 100ML IV/TID
-INJ PAN 40MG IV/BD
-INJ ZOFER 4MG IV/SOS
-INJ OPTINEURON 1amp in 100ml NS IV/OD
-TAB PCM 650MG TID
-TAB CHYMORAL FORTE TID
-Strict I/O Charting












Comments
Post a Comment